Billing Services for your Large Practice
Doctors Medical Center and Large Practices Share Common Goals

Accelerated Cash Flow

Precision in Billing and Coding

Enhance Patient Experience

Comprehensive Denial Management

Regulatory Compliance

Cost Efficiency
A Robust Billing Infrastructure: A Key Feature of Our Medical Billing Services
Large practices encounter numerous challenges, from patient registration to claims submission and follow-up. Among these, managing multiple claims stands out as a significant struggle amidst various administrative burdens.
A robust billing infrastructure ensures transparency, affordability, and flexibility, addressing weaknesses in billing processes. At Doctors Medical Center, we excel in this area with efficient systems, up-to-date denial management resources, and a team of experienced professionals. Our services offer comprehensive solutions and 24/7 support to meet all your billing needs.
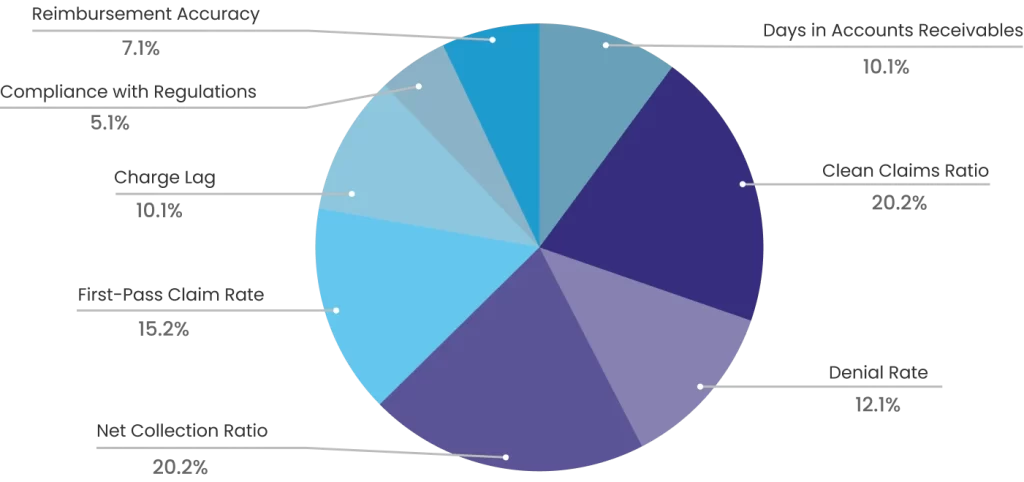
8 Important KPIs to Ensure Faster and Higher ROI
These metrics are crucial components of the revenue cycle management flowchart, essential for optimizing the billing process and overall financial performance of your large practice.
We Use 4 Key Metrics to Audit Billing and Enhance ROI for Your Large Practice
These metrics are crucial components of the revenue cycle management flowchart, essential for optimizing the billing process and overall financial performance of your large practice.
Days in Accounts Receivable - 30-40 Days
Accounts Receivable - This metric tracks the average number of days it takes for a practice to collect payments. We maintain a lower accounts receivable days ratio, ensuring quicker reimbursement and more efficient cash flow.
Net Collection Rate - 98%
The net collection rate reflects the total amount collected from both patients and insurers. We ensure timely payment processing to achieve a high net collection rate.
First Pass Acceptance Rate - 97%
This key performance indicator measures how many claims are accepted on their initial submission without needing corrections. Our comprehensive revenue cycle management services are designed to maximize this rate, leading to faster payments and fewer claim denials.
Denial Rate - 1%
The ratio of claims denied by the insurer indicates the effectiveness of your revenue cycle management process. We proactively follow up on denied claims, identify and correct errors, and work to maximize revenue generation.
Unlock Personalized Medical Billing Services to Elevate Your Billing Accuracy, Coding Efficiency, and Revenue Cycle Management
We recognize that one size does not fit all, and your large practice requires tailored services that are both transparent and error-free. We meticulously audit your billing process, identify and correct errors, and review all unpaid and aging claims to ensure accuracy and efficiency.
Your large practice faces numerous challenges, from patient registration to claims submission and denial management. We handle all your non-clinical tasks, allowing you to concentrate on providing exceptional patient care.
We have established comprehensive billing, coding, and RCM systems tailored for your large practice. We achieve a clean claim submission rate of over 99%, ensure timely filing of medical claims, diligently follow up on aging accounts receivable daily, and work to maximize reimbursements.

Medical Billing Services to Streamline Revenue Cycle Management for Large Practices
Simplify the complexities of medical billing and boost your financial and healthcare productivity by implementing the following billing flowchart for your large practice.

Insurance Verification and Eligibility
Verify insurance eligibility and secure prior authorization for medical services, including diagnoses, procedures, and treatments.

Patient Registration
Collect, verify, and input data into the system to ensure accurate and error-free billing documentation.

Claims Submission
With a 99% clean claim rate, we submit accurate claims to achieve a high first-time pass rate, ensuring you receive the maximum collection rate.

Coding and Documentation
We utilize expert coders and billers to prevent errors and inaccuracies in diagnostic and procedural coding.

Denial Management
Addressing the root cause of denials ensures accuracy and effective denial management.

Payment posting
Payments received from insurers or patients are recorded in the system for accurate record-keeping and to notify patients of any outstanding co-pays.

A/R Follow-up
We diligently track and manage pending payments and accounts receivable to ensure timely reimbursements and complete the remaining collections.

Patient Billing
Patients are billed accurately to cover the costs of the services they have received.

Education and Outreach
Through proactive collaboration with providers, we ensure a clear understanding of patients' financial responsibilities, encouraging prompt payment.
Our Efficient Work Process to Achieve These Goals Faster
24/7 Access to Technology and Infrastructure
State-of-the-art billing technology, advanced coding tools, and robust infrastructure are integral to efficiently managing operations and customizing billing and RCM services for large practices. When you partner with Doctors Medical Center for your billing needs, you benefit from these sophisticated resources without incurring the costs associated with software or hardware investments.


Regular Auditing and Quality Control
We conduct regular internal audits to identify inaccuracies and highlight areas for improvement within the billing processes. Additionally, we address recurring issues and implement stringent quality control measures, including double-checking claims and performing thorough reviews. These practices help to minimize revenue losses and enhance accuracy.
Upfront Communication
Clear and effective communication between insurers, administrative staff, and billing personnel is crucial for building long-term partnerships. It fosters trust among all parties involved and helps prevent misunderstandings and errors.


Expertise and Specialization
Experience and professionalism are crucial for minimizing denials. Our team of skilled experts, trained in coding, billing, and claims submission, ensures compliance and accuracy. Your large practice can leverage this expertise to enhance billing practices and reduce denials.
Simplifying Complex Coding System (ICD-10, CPT, HCPCS)
We stay current with the latest regulatory changes, coding guidelines, and insurance requirements. Our coders are proficient in ICD-10, CPT, and HCPCS coding systems, ensuring accuracy and accelerating collections.

