Denial Management Services
Remove Claim Denials Root and Stem Because All Denials Are Preventable.
- 100+ Denial management experts skilled in state, federal, and commercial payers.
- Resolve soft, hard, clinical, and administrative denials.
- Reduce denials with our analytics expertise.
- Denial management system.
- Automated denial management services.
Save time, money, and energy by outsourcing the denial management service.
Quick Inquiry Form
Who we serve?
Eligibility and Authorization Denials
These occur when a patient’s insurance coverage is not verified before treatment or when prior authorization for a service is missing. Effective management involves verifying eligibility and obtaining necessary authorizations before service delivery.
Coding and Billing Errors
Claims are denied due to incorrect coding, such as improper diagnosis or procedure codes. Managing these denials requires accurate coding and ensuring compliance with payer guidelines to reduce errors.
Missing or Incomplete Information
Denials arise when critical claim information, such as patient details or medical documentation, is missing. Ensuring thorough documentation and double-checking claims can help prevent these errors.
Timely Filing Denials
Insurers reject claims not submitted within their required timeframe. A proactive approach with regular monitoring of submission deadlines and follow-up ensures claims are filed promptly to avoid such denials.
Our Denial Management Service Workflow
Denial Manager gives complete and immediate visibility into each claim and denial
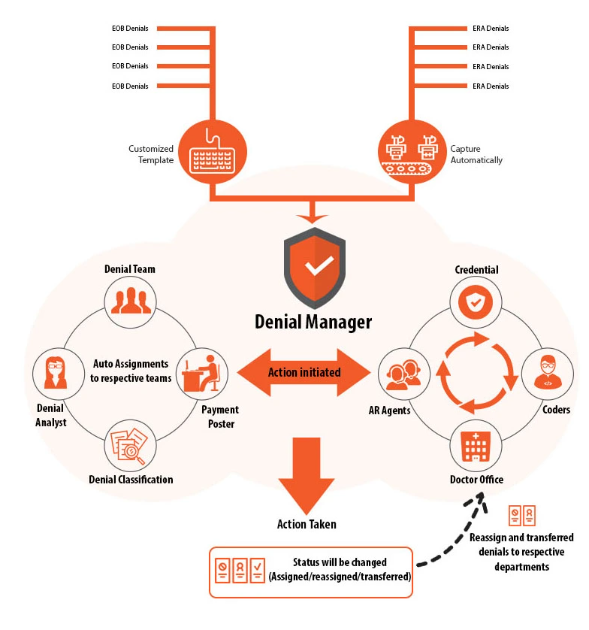
Our Denial Management Service Workflow is a systematic approach aimed at minimizing revenue loss due to denied claims. It begins with a detailed review and analysis of the denied claims to identify the root causes, such as coding errors, documentation gaps, or insurance-related issues. We then categorize the denials by type, such as eligibility, coding, or timely filing errors. Based on this categorization, we implement corrective actions to resolve the issues efficiently. Finally, we resubmit the claims and track their status to ensure successful reimbursement, continuously improving the process to reduce future denials.
Denial Management FAQs
This term represents the act of appealing and managing denial claims that can occur due to numerous reasons.
A claim denial can occur due to many reasons, the most prominent of which include errors in eligibility verification and breakdown of benefits or using wrong codes for the charge entry of a specific treatment offered.
Whether it is your internal practice medical billing or family practice medical billing, the top 5 denials are the following:
- Denial as a result of missing information in any field.
- Expired limit for filing.
- A duplicate service or claim.
- Denial when the service is not covered by the payer.
- Denial when a service is already adjudicated.
- Denial management is a domain in medical billing that caters to the claim denials occurring in the revenue cycle. However, account receivables includes all claim denial and unfiled claims that are yet to be received by the medical practice from the patients or the insurance networks.
Doctors Medical Denial Management Service Results
72%
Decrease in the denial rate.
45%
Reduced operational costs.
32%
Reduction in DNFB accounts.
72%
Productivity improvement.
36%
Reduction in aged A/R.
98%
Achieve net collections.
The Denial Management tool algorithm analyzes the denied claim under the following protocols
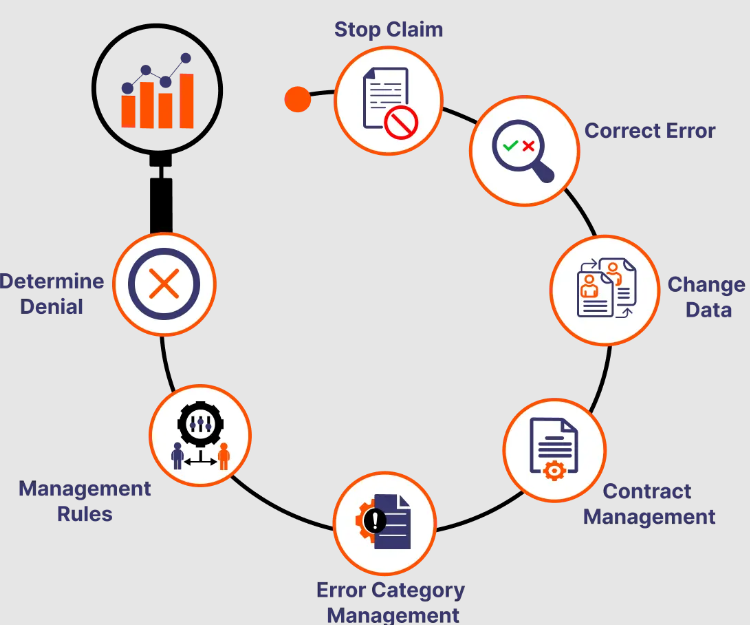
Appeal Automation
Appeal forms for most of the payers are listed. If the required appeal form it is uploadable?
Denied claim information is automatically populated in the appeal form.
Appeal Automation
Appeal forms for most of the payers are listed. If the required appeal form it is uploadable?
Denied claim information is automatically populated in the appeal form.
Conclusion
To conclude, one can claim that A/R management is a core aspect of revenue cycle management. This is why I-Med Claims LLC is focused to provide optimum RCM billing services to make sure your account receivables are always under control, and you are able to collect maximum revenues through prompt claim reimbursements. Such an approach is vital to maintaining a smooth workflow that enables practices to perform at their best.
I-Med Claims LLC is a professional medical billing company that specializes in all steps of the revenue cycle. This is why we are offering end-to-end revenue cycle management, which means that we’ve got you covered completely in a number of ways. You can easily manage your claim denials by partnering with the denial management experts and consultants working at I-Med Claims LLC.
Ready to Talk to our Denial Management experts?
Call us today to streamline your billing and revenue cycle. Let Doctors Medical Center handle the complexities, so you can focus on patient care. Reach out now for a personalized consultation!
